Kale: The Dangerous
How many unreferenced blogs have you come across warning you that kale, and other vegetables from the brassicae family, are, in fact, dangerous and interfere with thyroid functions and its hormones?
On the other hand, pro-organic and nutritional experts claim that brassicas (once called green leafy vegetables, or cruciferous) should be eaten at every meal, for they are topping the list of nutrient-dense foods. These foods are ranked according to how many nutrients they supply compared to their calorie content.
Brassicas, including kale, are packed with key minerals, especially magnesium, vitamins, essential fatty acids, enzymes, compounds that have antioxidant properties, and others that are useful in detoxification, and much much more.
How could kale be labelled as dangerous?
It will always surprise me how some studies are conducted to create news headlines, and how many people will jump on the wagon, spreading what they have “uncovered” without thorough research of their own.
The farce on cholesterol and fat is the perfect example of how a lie can enter the government association circles and make it to the top of their agendas.
It is obvious that giving fat to a rabbit (because everyone knows a rabbit is a carnivore and loves fat) is useful in human studies, right? And, as a result, cholesterol in the blood of the rabbit rises and this leads to cardiovascular risk in humans. The link is indisputable… This is what we were told for decades until the lies were exposed
But what has this to do with Kale?
Goitrogens were identified nearly a century ago (1928).
It was uncovered that “goitrogens had an anti-carcinogenic effect. Despite the high spontaneous tumor incidence in a strain mice, during goitrogenic treatment such mice had no spontaneous tumors, even in old age.” (Gorbman, A. 1947. p. 756)
This is quite old news, and yet, brassicas only received widespread attention once the ANDI score was invented in the late 90s and taken on board by the likes of Wholefoods years later in the hope of helping people make better choice when shopping for food.
Kale has then become the queen of plants, scoring 1,000 on the ANDI scale, the maximum score possible.
When attention is given to something in particular there will always be the doubters and others who just want the attention to go away.
That we want it or not, any plant or herb exerts a therapeutic (medicinal) effect on the body. Like a medicine, some people can react to food or be susceptible to some of their compounds.
It has been long known that thyroid function is disturbed during pregnancy and that brassicas may exert a further goitrogenic effect on the thyroid, especially, if consumed in very large quantities.
What are goitrogens?
According to Thyroid UK: “Goitrogenic foods can act like an antithyroid drug in disabling the thyroid function. They prevent the thyroid from using available iodine. It is made worse if you use a lot of salt because that causes the thyroid to swell.
Here is a list of some goitrogens:
Brussels sprouts, rutabaga, turnips, cauliflower, cabbage and kale
Almonds, peanuts and walnuts
Sweetcorn, sorghum and millet
Soya: when combined with a high-fibre diet causes too much thyroid hormone and iodine to be excreted from the body
Raw Swedes, turnips and kale - These are sometimes fed to cattle and expose us to more goitrogens via their milk products.
“Cruciferous vegetables contain thioglucosides that are metabolised to thiocyanates. These compounds inhibit iodine transport and the incorporation of iodide into thyroglobulin, thus increasing TSH secretion and thyroid cell proliferation.
“In animal experiments, it has been found that these substances induce thyroid carcinomas. Another group of potent goitrogens are contained in food such as cassava or sweet potatoes, with a high content of cyanogenic glycosides. In epidemiological studies, no clear association between thyroid cancer and cruciferous vegetables or other food items containing goitrogens has been demonstrated.” (Truong, T. et al. 2010. p. 1184)
Goitrogens are compounds that interfere with the normal function of the thyroid gland, disturbing hormone production, and it closely linked to iodine (excess or deficiency).
There are four types of goitrogens:
Goitrins
Nitriles
Thiocyanates
Flavonoids
Goitrins, nitriles and thiocyanates are the result of chemical reactions when plants are damaged, such as when they are sliced or chewed, creating glucosinates, a plant self-defence mechanism (pesticide).
Glucosinolates are broken down in our body during digestion into goitrogenic and non-goitrogenic compounds.
Flavonoids are naturally present in a wide variety of foods and have antioxidant properties, but some of them can be converted into goitrogenic compounds by our gut bacteria
Are goitrogens a concern to human health?
There is only one reported case in the world of thyroid dysfunction because of brassica intake. In this particular case, the person was consuming exceptionally excessive doses every single day (several kilos).
And this is from this incident that today kale is Mankiller!
You may need to worry about goitrogens if you suspect or were diagnosed with thyroid dysfunction, or if you are pregnant or nursing.
The other great danger is that many people are not aware that they have thyroid problems, because symptoms are so broad (stress, fatigue, poor memory and concentration, weight gain, etc.) and need to watch any foods that can impact their thyroid, and those include gluten too.
Which food have the highest content of goitrogens?
A surprising variety of foods contain goitrogens, including vegetables, fruits, starchy plants and soy-based foods.
How do problems start?
For people with thyroid problems, coupled with iodine deficiency, high intake of goitrogens can disturb thyroid function even further by:
Blocking iodine (goitrogens interfere with iodine uptake in the thyroid gland, which is needed to produce thyroid hormones).
Interfering with the Thyroid Peroxidase (TPO) enzyme attaches iodine to the amino acid tyrosine to form thyroid hormones.
Reducing TSH: Goitrogens may interfere with thyroid stimulating hormone (TSH), which helps the thyroid gland produce hormones.
Thyroid dysfunction can lead to symptoms linked to energy and metabolism: body temperature, heart rate, protein production, use of fat and carbohydrates for energy, with an increased risk for weight gain, obesity, heart disease, metabolic syndrome, liver and gallbladder dysfunction, and cognitive decline.
The body’s response is to release more TSH. The thyroid gland responds to TSH by making more hormones and, if it cannot keep up, compensates by growing more cells, leading to an enlargement known as a goitre.
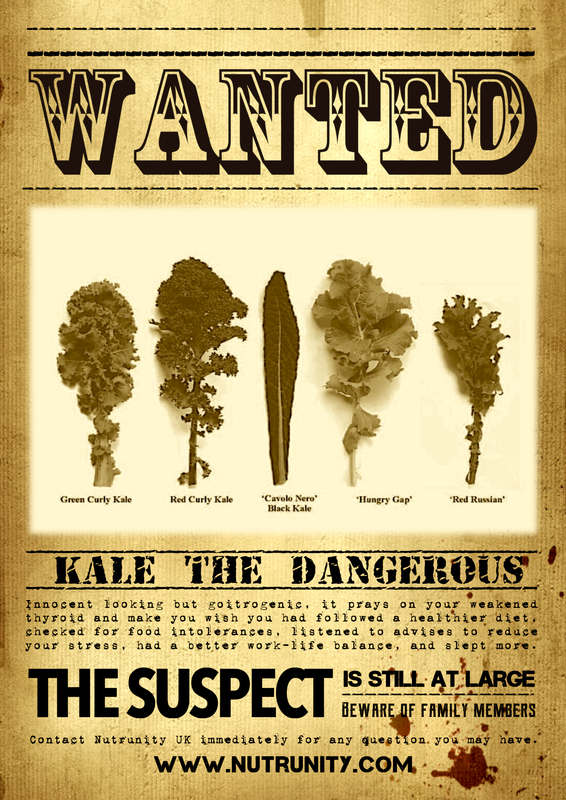
Certain varieties of kale are the biggest goitrogenic offenders, together with collards and Brussels sprouts, so there is reason to minimise their intake if you suffer from thyroid problems, are at risk of iodine deficiency, or are pregnant or nursing.
It is also important to note that thyroid dysfunction occurs because of gut and widespread inflammation, often due to food sensitivities, sugar-rich diet, regular alcohol intake, foods that may induce an immune response, and an omega-6-rich diet.
A very-low carbohydrate and a low-protein diet can interfere with thyroid hormone because it requires insulin to covert T4 to T3 (active thyroid hormone).
Many environmental chemicals and medications are also classified as goitrogenic:
Amiodarone (medication for irregular heart beat)
Antibiotics
Bromides (from pesticides, plastic, brominated vegetable oils, medications)
Dioxins (toxic industrial byproducts)
Heavy metals
NSAIDs
Lithium and benzodiazepines (depression and anxiety drugs)
Oxazolidines (from paint)
Perchlorates (from jet fuel, water)
Pesticides
Thiocyanate (in cigarettes)
Oxalates can also present another problem for people with thyroid disorders. Oxalates are compounds naturally found in plants and are able to bind to minerals preventing them from being assimilated by the body.
Because thyroid dysfunction starts in the gut (dysbiosis, gut inflammation, food sensitivities, etc.), it often reveals an unbalanced gut microflora (dysbiosis). Oxalates are broken down by gut bacteria, but when our gut microflora is compromised, oxalates can enter the bloodstream and turn into crystals ending in kidney tissue (kidney stones).
So, is kale dangerous?
The answer is not really.
Goitrogens are not an outright death sentence. When cooked and consumed in moderation, Kale, and other members of the brassica family, should be safe for everyone — even those with thyroid problems. To be sure, contact us or your health practitioner.
If you follow a healthy diet, eat little processed food and a wide range of colourful fruits and vegetables, and exercise as often as you can, there will be little chance of having issues with your thyroid, especially if you avoid foods susceptible to generating inflammation, such as alcohol, sugar, and food known to disturb your gut integrity and bacterial microflora (gluten, dairy, oxalates and phytates).
Cooking lowers the goitrogenic content of food. Often, I recommend lightly steaming green leafy vegetables to preserve all the nutrients, but you may boil them further if you have thyroid problems, and limit your intake to one serving per day if you have hypothyroidism. And of course, it is all about moderation. Anything in excess is bound to create issues.
AVOID drinking many green juices made with raw cruciferous and, especially, spinach (very high in oxalates), and AVOID eating brassicas raw.
"Fermenting increases the goitrogen content of cabbage, but it simultaneously decreases the level of nitriles. Because nitriles are more harmful than goitrogens, the overall effect of fermentation is probably positive," explains Kris Kresser*
Make sure you ingest enough iodine every day to prevent deficiency and multiply the goitrogenic effect of kale and other vegetables from the brassica family.
Other effective Strategies to improve Thyroid function
The most important factor when it comes to thyroid dysfunction is inflammation. Usually, this is the result of gut inflammation, bad oral care, food intolerances, high intake of sugar and alcohol, chronic stress and a disproportionate stress response, anxiety and depression.
Mastering blood sugar in these cases is essential.
Heal your gut. Remember that gut bacteria assist to convert T4 to T3.
Check your Vitamin D level and maximise safe sun exposure. Vitamin D is involved in immune function and autoimmunity. Hypothyroidism is often the result of autoimmunity, a cross-reaction with the molecule of gluten in particular.
Exclusively opt for Organic or Biodynamic food and avoid ultra-processed and refined foods as much as possible. This will also help you reduce your intake of toxins.
Make sure you consume enough selenium-rich foods.
Eat a varied, balanced diet.
The last word
(Knusden, N. et al. 2002. p. 879)
Abstract:
"The occurrence of thyroid diseases is determined by interplay between genetic and environmental factors. The major environmental factor that determines goiter prevalence is iodine status, but other environmental factors influencing entire populations have been identified such as goitrogens in food and drinking water.
Less focus has been on individual environmental factors and the interplay between factors. The goiter prevalence is higher in certain groups in the population. The variation in goiter prevalence between the genders is well known with a higher occurrence among women. The association with age is probably dependent on iodine status, because it seems that the zenith of goiter prevalence appears earlier in life the more severe iodine deficiency the population is exposed to.
The association with individual risk factors has been investigated in some studies, especially the association with tobacco smoking. In iodine-deficient areas, a strong association between tobacco smoking and goiter prevalence is found, whereas the association is less pronounced in iodine-replete areas. This was predictable from experimental studies showing thiocyanate to be the mediator of the goitrogenic effect of tobacco smoke acting as a competitive inhibitor of iodine uptake. The association with alcohol intake has only been investigated in few studies, but a low occurrence of goiter among alcohol consumers has been found. The mechanism of this association is not known.
Increased goiter prevalence during pregnancy has been reported, and recently a long-term goitrogenic effect of pregnancies has also been shown. As demonstrated for tobacco smoking, this association is dependent on iodine status, because the association has only been found in areas with a suboptimal iodine intake. This indicates pregnancy-induced goiter to be the result of exacerbation of existing iodine deficiency.
[…] Some implications for prevention of thyroid disease could be suggested. Discussion of smoking habits should be included in a consultation for goiter with a motivation to quit smoking. Iodine deficiency has particularly strong goitrogenic effects during pregnancy and for the sake of the mother as well as the fetus, sufficient iodine supply should be ensured to all pregnant women. The difference in age maximum in goiter prevalence suggests that monitoring of iodine deficiency disorders should ideally include a spectrum of age groups."
Tip: Stop smoking!
(click on this link for help)
References
Andersson, M. Karumbunathan, V. Zimmermann, MB.. (2012). Global iodine status in 2011 and trends over the past decade. The Journal of Nutrition. 142 (4), pp. 744–750.
Boeing, H. et al. (2012). Critical review: vegetables and fruit in the prevention of chronic diseases. European Journal of Nutrition. 51 (6), pp. 637–663.
Chandra, AK. Mukhopadhyay, S. Lahari, D. Tripathy, S. (2004). Goitrogenic content of Indian cyanogenic plant foods & their in vitro anti-thyroidal activity. The Indian Journal of Medical Research. 119 (5), pp. 180–185.
De Herder, WW. et al. (1989). On the enterohepatic cycle of triiodothyronine in rats; importance of the intestinal microflora. Life Science. 45 (9), pp. 849–856.
De Souza Dos Santos, MC. et al. (2011). Impact of flavonoids on thyroid function. Food and chemical Toxicology: an international journal published for the British Industrial Biological Research Association. 49 (10), pp. 2495–2502.
Dolan, LC. Matulka, RA. Burdock, GA. (2010). Naturally Occurring Food Toxins. Toxins. 2 (9), pp. 2289–2332.
Duntas LH. (2010). Selenium and the thyroid: a close-knit connection. The Journal of Clinical Endocrinology and Metabolism. 95 (12), pp. 5180–5188.
Eastman, CJ. Zimmermann, MB. (2018). The Iodine Deficiency Disorders. Endotext. (internet). Available at: https://www.ncbi.nlm.nih.gov/books/NBK285556/. Last accessed: August 5th 2018.
Felker, P. Bunch, R. Leung, AM. (2016). Concentrations of thiocyanate and goitrin in human plasma, their precursor concentrations in brassica vegetables, and associated potential risk for hypothyroidism. Nutrition Reviews. 74 (4), pp. 248–258.
Finkielstein, VA. Goldfarb, DS. (2006). Strategies for preventing calcium oxalate stones. Canadian Medical Association Journal. 174 (10), pp. 1407–1409.
Fox, CS. et al. (2008). Relations of thyroid function to body weight: cross-sectional and longitudinal observations in a community-based sample. Archives of Internal Medicine. 168 (6), pp. 587–592.
Kathleen, L. et al. (2013). Iodine Status in Pregnant Women in the National Children's Study and in U.S. Women (15–44 Years), National Health and Nutrition Examination Survey 2005–2010. Thyroid. 23 (8), pp. 927–937.
Knudsen, N. et al. (2002). Risk factors for goiter and thyroid nodules. Thyroid. 12 (10), pp. 879–888.
Mccarrison, R. (1933). A Paper on FOOD AND GOITRE. British Medical Journal. 2 (3797), pp. 671–675.
Ochs, N. et al. (2008). Meta-analysis: subclinical thyroid dysfunction and the risk for coronary heart disease and mortality. Annals of Internal Medicine. 148 (11), pp. 832–845.
Onigata, K. (2014). Thyroid hormone and skeletal metabolism. Clinical Calcium. 24 (6), pp. 821–827.
Pasqualetti, G. et al. (2015). Subclinical hypothyroidism and cognitive impairment: Systematic review and meta-analysis. The Journal of Clinical Endocrinology and Metabolism. 100 (11), pp. 4240–4248.
Rungapamestry, V. et al. (2007). Effect of cooking brassica vegetables on the subsequent hydrolysis and metabolic fate of glucosinolates. The Proceedings of the Nutrition Society. 66 (1), pp. 69–81.
Singh, S. et al. (2008). Impact of subclinical thyroid disorders on coronary heart disease, cardiovascular and all-cause mortality: a meta-analysis. International Journal of Cardiology. 125 (1), pp. 41–48.
Stagnaro-Green, A. Pearce, EN. (2013). Iodine and pregnancy: a call to action. Lancet. 382 (9889), pp. 292–293.
Sullivan, KM. et al. (2013). Monitoring the Iodine status of pregnant women in the United States. Thyroid. 23 (4), pp. 520–521.
Tolonen, M. et al. (2002). Plant-derived biomolecules in fermented cabbage. Journal of Agricultural and Food Chemistry. 50 (23), pp. 6798–6803.
Vanderpas, J. (2006). Nutritional epidemiology and thyroid hormone metabolism. Annual Review of Nutrition. 26, pp. 293–322.
*https://kresserinstitute.com/