Chronic Intake of Food Additives Leads to Marked Changes via the Microbiota-Gut-Brain Axis.
In addition to discovering from previous articles that food additives are largely toxic, with severe adverse effects, including immune hyperreactivity and systemic inflammation, it's important to note that the impact of food additives extends much further. They may also contribute to neuroinflammation and neurodegeneration, potentially paving the way for disorders like dementia and Alzheimer's.
A study published in the journal Toxicology in 2021 was really interesting because it looked at the interconnectivity between the gut and the brain, but also the role the gut microbiota plays in the conversation and in the pathogenesis of many diseases.[1] Additionally, they looked at food additives and their impact on the gut microbiome and the gut-brain axis.
The main finding of the systematic interpretative literature review is a clear link between the changes in the gut microbiota promoted by food additives and the causes that lead to many reported diseases related to chronic food additives consumption.
The team behind the study, Pilar Abiega-Franyutti and Veronica Freyre-Fonseca, aimed to clarify how food additive-triggered gut dysbiosis and gastrointestinal disorders affect the microbiota-gut-brain axis.
A meticulous literature review was conducted across seven academic search engines, revealing a conspicuous correlation between alterations in gut microbiota induced by food additives and the onset of various chronic diseases associated with chronic food additive consumption. Despite these findings, research on additive effects remains inadequate, highlighting the need for future investigations in this domain and better monitoring.
Introduction
During the last decades, the food industry has developed ingenious ways to produce new food products using cheap and poorly nutritious ingredients and yet made those extremely addictive using the power of cleverly designed food additives. These include dyes, foaming agents, stabilizers, emulsifiers, flavour enhancers and many more. Notably, synthetic colourants, emulsifiers and sweeteners have been implicated in behavioural changes and dysbiosis, ultimately affecting the microbiota-gut-brain axis.
Microbiota-Gut-Brain Axis
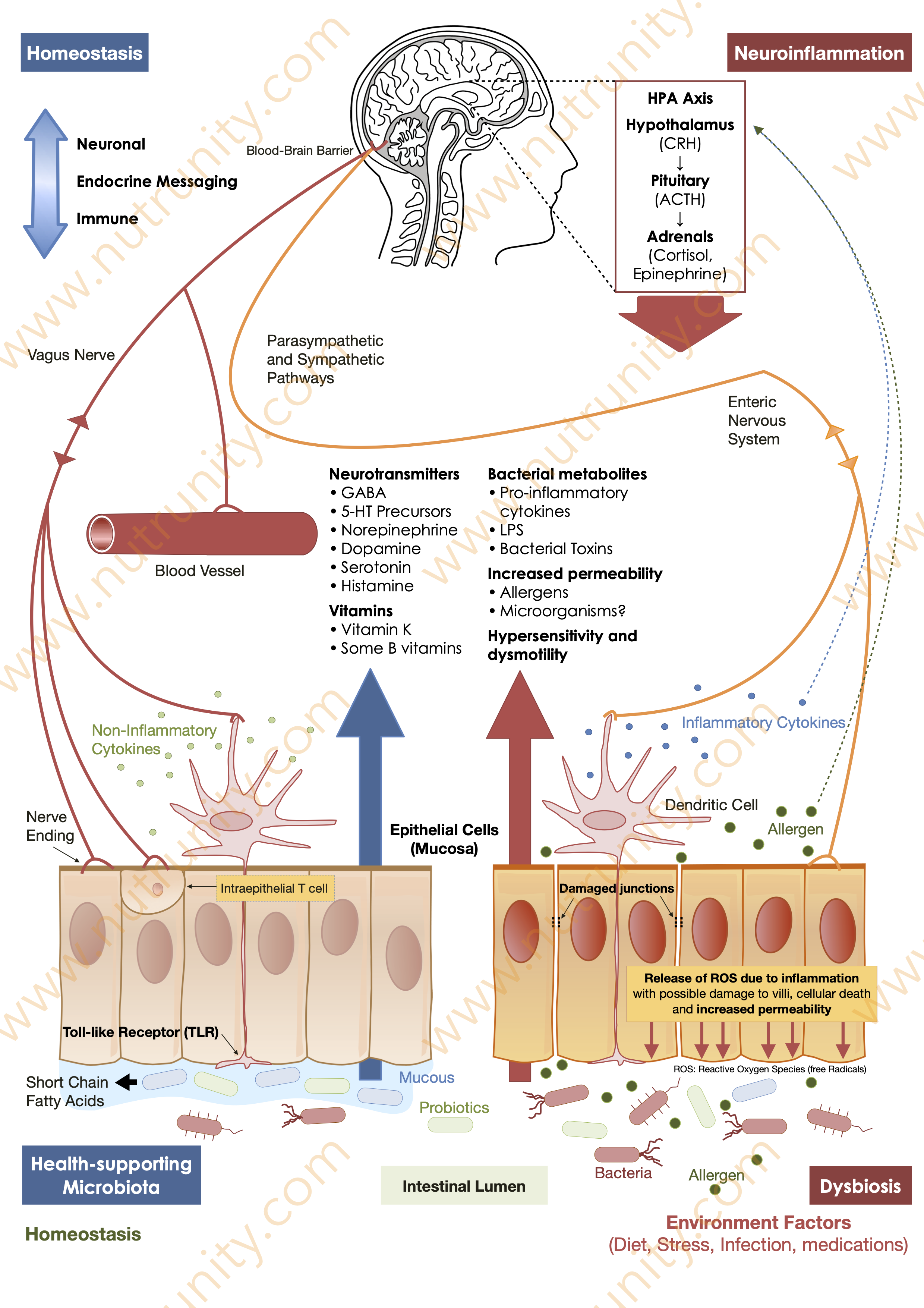
The human gastrointestinal tract harbours a diverse microbiota crucial for functions like nutrient absorption, immune modulation, and neurotransmitter regulation. As microbiota mature, they influence metabolic processes and maintain homeostasis through short-chain fatty acids (SCFAs). Dysbiosis, triggered by factors like food additives, can disrupt this delicate balance, potentially leading to inflammatory responses and chronic diseases.
Schematic representation of the microbiota-gut-brain axis, dysbiosis, increased intestinal permeability, and neuroinflammation, via the release of neurotransmitters, short-chain fatty acids, and either anti- or pro-inflammatory cytokines. Illustration by Sanchez, O. (2021). Energise - 30 Days to Vitality. p. 25.
Immunological Responses
The Gut-Associated Lymphoid Cell (GALT) plays a vital role in protecting the gut from pathogens. Dysbiosis can compromise GALT function, leading to unregulated immune responses and inflammation. Increased expression of the NOD2 protein, associated with additive consumption, may exacerbate inflammatory conditions such as Crohn's disease and inflammatory bowel disease (IBD).
Intestinal Peptides and Hormones
The gut houses enteroendocrine cells, which release peptides in response to stimuli, influencing appetite, stress, and immune responses.
Neuropeptides, like phoenixin and vasoactive intestinal peptides, contribute to various physiological functions, demonstrating the intricate communication between the gut and the central nervous system.
“There is currently a high consumption of ultra-processed foods, some of these have negative effects on microbiota. Some food preservatives like sodium benzoate, sodium nitrite or potassium sorbate, sweeteners, emulsifiers and synthetic colorants; have been shown to induce behavioral changes as well as dysbiosis.”
Neuropeptides
Neuropeptides are small protein-like molecules that function as signalling molecules in the nervous system. They are produced by neurones and play a crucial role in neural communication.
Neuropeptides act as neurotransmitters or neuromodulators, influencing the activity of other neurones. These molecules are involved in a wide range of physiological processes, including the regulation of mood, pain perception, stress response, and various aspects of behaviour.
Neuropeptides can have diverse effects on the central nervous system and peripheral tissues, contributing to the complex network of signalling within the nervous system.
It is recognised that up to 90% of the serotonin, the so-called ‘feel good’ neurotransmitter, found in the body is produced by the gut. However, gut-produced serotonin cannot enter the brain as too big a molecule. Neuropeptides produced in response to serotonin will take on that role and, therefore, impact brain function and various physiological processes.
Food Additives and Dysbiosis
Specific additives, such as emulsifiers (carboxyl methylcellulose and polysorbate 80), sweeteners, and synthetic colourants, have been associated with dysbiosis. For instance, emulsifiers may promote the pathogenesis and progression of chronic inflammatory gut diseases by altering the gut bacterial composition, leading to increased production of pro-inflammatory factors.[2] (see illustration above)
Neuroinflammation and Ultra-Processed Products
Recent studies indicate a strong association between the consumption of ultra-processed foods and neuroinflammation. These foods, rich in artificial additives, may trigger inflammatory responses in the brain. The link between chronic inflammation and neurodegenerative diseases, such as Alzheimer's and Parkinson's, is becoming increasingly evident.[3]
Gut-Brain Axis Disruption
Ultra-processed food products disrupt the delicate balance of the gut-brain axis, influencing communication between the microbiota and the central nervous system. This disturbance may contribute to mood disorders, anxiety, and cognitive decline.[4,7]
The gut-brain axis is a bidirectional communication network connecting the central nervous system (CNS) and the enteric nervous system (ENS). This communication involves neural, hormonal, and immunological signalling. The gut microbiota, comprising trillions of microorganisms, plays a crucial role in this axis.
The gut microbiota communicates with the CNS through the release of metabolites, neurotransmitters, and inflammatory mediators. Ingesting ultra-processed foods can alter the production of these signalling molecules, potentially leading to aberrant neural responses. For instance, changes in neurotransmitter levels (e.g., serotonin) due to microbiota alterations can influence mood regulation.[5]
Disruptions in the gut-brain axis have been implicated in mood disorders like depression and anxiety. The altered microbial profile in response to a diet rich in ultra-processed foods may contribute to the release of stress hormones and inflammatory factors. Chronic inflammation, triggered by dysbiosis, has been linked to the development and exacerbation of mood disorders.[6]
The mechanisms through which ultra-processed food products impact the gut-brain axis are multifaceted. They include direct effects on neurotransmitter synthesis, modulation of inflammation, and alterations in the permeability of the gut lining. All of these factors affect brain function, induce neuroinflammation and affect mood and cognitive dysfunction.[8]
In summary, the disruption caused by ultra-processed foods in the delicate balance of the gut-brain axis can lead to changes in neural signalling, inflammation, and gut permeability. These disturbances may contribute to the development or exacerbation of mood disorders, anxiety, and cognitive decline. A diet focused on maintaining a healthy gut microbiota through whole, minimally processed foods is increasingly recognized as a key element in promoting both gastrointestinal and neurological well-being.
Additives and Oxidative Stress
Certain additives in ultra-processed foods, such as artificial colourants and emulsifiers, have been linked to increased oxidative stress in the brain. Oxidative stress is a known factor in neurodegenerative conditions. Antioxidant-rich diets, in contrast, may offer protective effects against the damage caused by these additives.[9]
For instance, Allura Red (E129), a widely used red food dye, has been associated with oxidative damage due to its potential to generate free radicals. Oxidative stress can harm neurones and is implicated in the progression of neurodegenerative disorders.
Food colourings are also linked to hyperactivity disorders, a link demonstrated since the 1970s.[10-12]
Aspartame, an artificial sweetener frequently used in diet products, has been investigated for its effects on cognitive function. Some studies suggest that excessive consumption of aspartame may lead to cognitive impairment, possibly through mechanisms involving oxidative stress.[13]
MSG, or Monosodium glutamate, a common flavour enhancer, has been studied for its potential impact on neurological health. While most research focuses on its role in headaches (Chinese Restaurant Syndrome), emerging studies suggest a connection between MSG and oxidative stress, indicating a need for further exploration into its effects on brain health.[14-16] Interestingly, animal studies show that curcumin appears to negate this effect.[17]
Sodium nitrite, a preservative often used in processed meats, has raised concerns regarding its potential neurotoxic effects. Animal studies indicate that nitrites may induce oxidative stress in the brain, leading to neuronal damage.[18]
Titanium dioxide nanoparticles (TiO2 NPs), used as a whitening agent, have been linked to neuroinflammation. Research suggests that TiO2 NPs may induce oxidative stress and neuroinflammatory responses in the brain, potentially contributing to the development or exacerbation of neurodegenerative conditions.[19-23]
Cognitive Decline and Dietary Patterns
Long-term adherence to diets dominated by ultra-processed foods has been associated with a higher risk of metabolic syndrome, inflammatory disorders and cognitive decline. Understanding the role of additives in compromising cognitive function sheds light on potential preventive strategies for neurodegenerative disorders.[24]
Diets high in ultra-processed foods often contain significant amounts of high-fructose corn syrup (HFCS), a common sweetener. Research suggests that excessive fructose intake, especially in the form of HFCS, may contribute to cognitive impairment. Elevated fructose levels have been associated with disruptions in synaptic plasticity, a key process in learning and memory.[25]
MSG has been linked to neuroinflammation. The excessive activation of glutamate receptors may contribute to neuronal damage and inflammation in the brain. This neuroinflammation is implicated in various cognitive disorders.[26]
Artificial sweeteners have been associated with blood sugar level disruption, weight gain, and cognitive impairment. They are also linked to liver and kidney dysfunction, and metabolic syndrome. Aspartame, for instance, is a widely used artificial sweetener that may affect neurotransmitter levels, potentially influencing cognitive function.[27,28] While there is much debate about the safety profile of artificial sweeteners such as aspartame, sucralose, acesulfame-K, and saccharine, evidence suggests that they and their accompanying metabolites may have neurotoxic effects. It is also possible that artificial sweeteners alter neurotransmitter synthesis and release, as well as induce oxidative stress, a cause of neuroinflammation and neurodegenerative disorders, such as Parkinson’s and Alzheimer’s.[29-33]
Emulsifiers, such as carboxymethylcellulose and polysorbate-80, commonly used in processed foods, have been shown to disrupt the gut-brain axis. This disruption may lead to alterations in microbial composition and inflammatory responses, potentially contributing to cognitive decline.
Emerging Research on Nanoparticles
Exploring the impact of food additive nanoparticles, such as titanium dioxide (TiO2), on gut microbiota, gut health and the subsequent influence on brain health is an area of ongoing research. Preliminary findings suggest a need for a closer examination of the effects of these nanoparticles on ulcerative colitis, colorectal cancer, and neurological functions.[34-36]
“We concluded that oral intake of anatase TiO2 NPs can induce neuroinflammation and could be neurotoxic and hazardous to health.”
While we may get an instant rush of dopamine upon eating (or drinking) ultra-processed, sugary products, those have been directly associated with depressive and anxiety disorders.[37] Would that be because with highs come lows and, that, with our constant pursuit of stimulation we end up entirely focussing on the lows and the things we lack?
“A meta-analysis of prospective studies demonstrated that greater ultra-processed food intake was associated with increased risk of subsequent depression. While we found evidence for associations between ultra-processed food consumption and adverse mental health, further [...] studies are needed to better understand causal pathways.”
By looking at the facts, we gain a more comprehensive understanding of how our dietary choices, especially regarding ultra-processed foods and their additives, can impact not only our gut health but also our brain function, our mood and overall well-being.
Time to break up from your addiction to sugar and domapine rush?
References
1. Abiega-Franyutti, P. Freyre-Fonseca, V. (2021). Chronic consumption of food additives leads to changes via microbiota-gut-brain axis. Toxicology. 464, 153001. doi:10.1016/j.tox.2021.153001
2. Narula, N. et al. (2012). Association of ultra-processed food intake with risk of inflammatory bowel disease: prospective cohort study. BMJ. 374, n1554. doi:10.1136/bmj.n1554
3. Badaeva, AV. et al. (2023). Perspectives on neuronutrition in prevention and treatment of neurological disorders. Nutrients. 15(11), 2505. doi:10.3390/nu15112505
4. Mörkl, S. et al. (2012). The role of nutrition and the gut-brain axis in psychiatry: A review of the literature. Neuropsychobiology. doi:10.1159/000492834
5. Cryan, JF. Dinan TG. (2012). Mind-altering microorganisms: The impact of the gut microbiota on brain and behaviour. Nature Reviews Neuroscience. 13(10), pp 701-12. doi:10.1038/nrn3346
6. Foster, JA. McVey Neufeld, KA. (2013). Gut-brain axis: How the microbiome influences anxiety and depression. Trends in Neuroscience. 36(5), pp. 305-312. doi:10.1016/j.tins.2013.01.005
7. Heneka, MT. et al. (2015). Neuroinflammation in Alzheimer's disease. Lancet Neurology. 14(4), pp. 388-405. doi:10.1016/S1474-4422(15)70016-5
8. Dinan, TG. Cryan, JF. (2017). The microbiome-gut-brain axis in health and disease. Gastroenterology Clinics of North America. 46(1), pp. 77-89. doi:10.1016/j.gtc.2016.09.007
9. Winiarska-Mieczan, A. et al. (2020). The role of dietary antioxidants in the pathogenesis of neurodegenerative diseases and their impact on cerebral oxidoreductive balance. Nutrients. 12(2), 435. doi:10.3390/nu12020435
10. Nigg, JT. et al. (2012). Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. Journal of the American Academy of Child and Adolescent Psychiatry. 51(1), pp. 86-97.e8. doi:10.1016/j.jaac.2011.10.015
11. Arnold, LE. Lofthouse, N. Hurt, E. (2012). Artificial food colors and attention-deficit/hyperactivity symptoms: Conclusions to dye for. Neurotherapeutics. 9(3), pp. 599-609. doi:10.1007/s13311-012-0133-x
12. Center for Science in the Public Interest. (2014). A summary of the science linking food dyes with impacts on children’s behavior. Available at: https://www.cspinet.org/sites/default/files/attachment/Food-Dyes-Fact-Sheet.pdf. Last accessed: November 11th, 2023.
13. Onaolapo, AY. Onaolapo, OJ. Nwoha, PU. (2017). Aspartame and the hippocampus: Revealing a bi-directional, dose/time-dependent behavioural and morphological shift in mice. Neurobiology of Learning and Memory. 139, pp. 76-88. doi:10.1016/j.nlm.2016.12.021
14. Pavlovic, V. et al. (2007). Effect of monosodium glutamate on oxidative stress and apoptosis in rat thymus. Molecular and Cellular Biochemistry. 303(1-2), pp. 161-166. doi:10.1007/s11010-007-9469-7
15. Banerjee, A. Mukherjee, S. Maji, BK. (2021). Worldwide flavor enhancer monosodium glutamate combined with high lipid diet provokes metabolic alterations and systemic anomalies: An overview. Toxicology Reports. 8, pp. 938-961. doi:10.1016/j.toxrep.2021.04.009
16. Liao, R. Wood, TR. Nance, E. (2020). Superoxide dismutase reduces monosodium glutamate-induced injury in an organotypic whole hemisphere brain slice model of excitotoxicity. Journal of Biological Engineering. 14:3. doi:10.1186/s13036-020-0226-8
17. Khalil, RM. Khedr, NF.(2016). Curcumin protects against monosodium glutamate neurotoxicity and decreasing NMDA2B and mGluR5 expression in rat hippocampus. Neurosignals. 24(1): pp. 81–87.
18. Landucci, E. et al. (2021). Neuroprotective effects of thymoquinone by the modulation of ER stress and apoptotic pathway in In vitro model of excitotoxicity. Molecules. 26(6), 1592. doi:10.3390/molecules26061592
19. de Oliveira Mallia, J. et al. (2022). Nanoparticle food applications and their toxicity: Current trends and needs in risk assessment strategies. Journal of Food Protection. 85(2), pp. 355-372. doi:10.4315/JFP-21-184
20. Ćwiek-Ludwicka, K. Ludwicki, JK. (2017). Nanomaterials in food contact materials; considerations for risk assessment. Roczniki Państwowego Zakładu Higieny [Annals of the National Institute of Hygiene]. 68(4), pp. 321-329.
21. Couto, C. Almeida, A. (2022). Metallic nanoparticles in the food sector: A mini-review. Foods. 11(3), 402. doi:10.3390/foods11030402
22. Mohammad, Z.H. et al.(2022). Application of nanotechnology in different aspects of the food industry. Discover Food. 2, Article number: 12. doi:10.1007/s44187-022-00013-9
23. McClements, DJ. Xiao, H. (2017). Is nano safe in foods? Establishing the factors impacting the gastrointestinal fate and toxicity of organic and inorganic food-grade nanoparticles. NPJ Science of Food. 1, 6. doi:10.1038/s41538-017-0005-1
24. Valls-Pedret, C. et al. (2015). Mediterranean Diet and age-related cognitive decline: A randomized clinical trial. JAMA Internal Medicine. 175(7), pp. 1094-1103. doi:10.1001/jamainternmed.2015.1668. Erratum in: JAMA Internal Medicine. 2018 Dec 1;178(12):1731-1732
25. Hsu, TM. el at. (2015). Effects of sucrose and high fructose corn syrup consumption on spatial memory function and hippocampal neuroinflammation in adolescent rats. Hippocampus. 25(2), pp. 227-239. doi:10.1002/hipo.22368
26. Rizzi, L. Rosset, I. Roriz-Cruz, M. (2014). Global epidemiology of dementia: Alzheimer's and vascular types. BioMed Research International. 2014:908915. doi:10.1155/2014/908915
27. Feijó, FM. et al. (2013). Saccharin and aspartame, compared with sucrose, induce greater weight gain in adult Wistar rats, at similar total caloric intake levels. Appetite. 60(1), pp. 203-207. doi:10.1016/j.appet.2012.10.009
28. Azeez, OH. Alkass, SY. Persike, DS. (2019). Long-term saccharin consumption and increased risk of obesity, diabetes, hepatic dysfunction, and renal impairment in rats. Medicina (Kaunas). 55(10), 681. doi:10.3390/medicina55100681
29. Sharma, A. et al. (2016). Artificial sweeteners as a sugar substitute: are they really safe? Indian Journal of Pharmacology. 48(3), pp. 237–240. doi:10.4103/0253-7613.182888
30. Maher, TJ. Wurtman, RJ. (1987). Possible neurologic effects of aspartame, a widely used food additive. Environmental Health Perspectives. 75, pp. 53–57.
31. Tandel, KR. (2011). Sugar substitutes: Health controversy over perceived benefits. Journal of Pharmacology & Pharmacotherapeutics. 2(4), 236–243. doi:10.4103/0976-500X.85936
32. Choudhary, AK. Lee. YY. (2018). Neurophysiological symptoms and aspartame: What is the connection? Nutritional Neuroscience. 21(5), 306–316. doi:10.1080/10284 15X.2017.1288340
33. Erbas, O. et al. (2018). Evaluation of long-term effects of artificial sweeteners on rat brain: A biochemical, behavioral, and histological study. Biochemical & Molecular Toxicology. 32(6), e22053. doi:10.1002/jbt.22053
34. Duan, S. et al. (2023). Oral intake of titanium dioxide nanoparticles affect the course and prognosis of ulcerative colitis in mice: involvement of the ROS-TXNIP-NLRP3 inflammasome pathway. Particle and Fibre Toxicology. 20(1), 24. doi:10.1186/s12989-023-00535-9
35. Barreau, F. et al. (2021). Titanium dioxide particles from the diet: involvement in the genesis of inflammatory bowel diseases and colorectal cancer. Particle and Fibre Toxicology. 18(1), 26. doi:10.1186/s12989-021-00421-2
36. Grissa, I. et al. (2016). The effect of titanium dioxide nanoparticles on neuroinflammation response in rat brain. Environmental Science and Pollution Research. 23(20), pp. 20205-20213. doi:10.1007/s11356-016-7234-8
37. Lane, MM. et al. (2022). Ultra-processed food consumption and mental health: A systematic review and meta-analysis of observational studies. Nutrients. 14(13), 2568. doi:10.3390/nu14132568