The impact of Adverse Childhood Experiences (trauma) in Adulthood
Is there a link between unresolved trauma and ill-health later in life? Could it be a trigger to develop behavioural patterns that impact your physical, mental and spiritual well-being at any stage of adulthood?
Can unresolved trauma impact your social skills, your relationship with your children and perhaps your marriage or other relationships as an adult?
Can adverse childhood experiences (ACEs) reduce your resilience and make you more prone to anxiety disorders and depression? Can it impact blood sugar, blood pressure and weight management? If so, is it an open door to metabolic disorders and neuroinflammation, thus leading to neurodegenerative diseases like dementia, including Alzheimer’s?
What does science show?
It seems that most scientists and researchers agree on one thing:
Unhealed childhood trauma can impact an adult at any time, including the relationships they may end up developing or avoiding.
Developmental trauma is more common than we are led to believe and, if you are close enough to someone, you may realise that they also have experienced trauma and that it may affect them in more than one way.
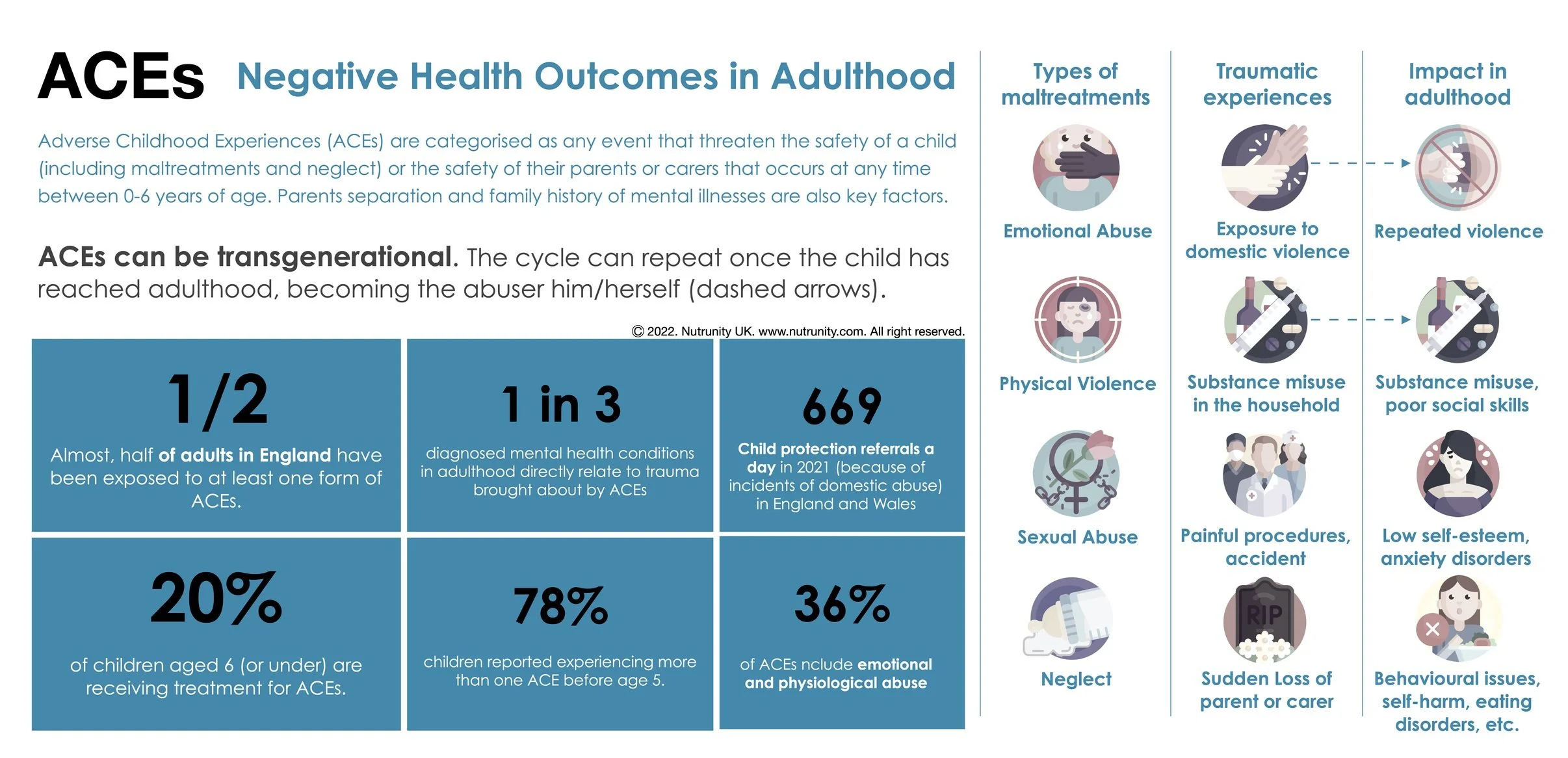
According to the National Child Traumatic Stress Network (NCTSN), 78% of children reported experiencing more than one adverse childhood event before age 5 and 20% of children aged 6 (or under) were receiving treatment for traumatic experiences, which may include neglect, domestic violence (witnessing or suffering), sexual abuse, and traumatic loss or bereavement.
This can carry well into the teenage years and also in adulthood and dependence on antidepressants is a leading factor to poor resilience and a complete lack of coping mechanisms at any time thereafter. In fact, a multitude of children continues to be prescribed antidepressants for decades. Teenage girls may also be given hormone therapy (OCP) to deal with period problems and hormonal imbalances.
The use of antidepressants may be justified since adults who suffered childhood trauma may go on to develop Complex Post Traumatic Stress Disorder (cPTSD). CPTSD is characterised by difficulties regulating emotions, concentration and memory and other types of cognitive dysfunction, such as brain fog, poor judgment and addictive behaviours; difficulties in building lasting relationships with other people; and a loss of purpose (living life in the passenger seat). Self-isolation and rumination are very common, feeding a very vicious circle with ill-health as an end product.
According to the CDC, in 2012 there were 3.4 million referrals to state and local child protective services for cases of abuse or neglect. 686,000 children were victims of maltreatment — 27% were younger than 3 years, and 20% were aged 3-5 years. Children younger than 1 year had the highest rate of victimisation.[1]
These numbers are solely for the US, so the global estimates may be very frightening indeed and the real impact on those children once they reach adulthood may be impossible to fathom.
As a result of the orchestrated global pandemic, UNICEF has established a report to record its achievements in helping children across the world; however, it also claims that “continued school closures, disruptions in health, social- and child protection and other services, compounded by caregiver sickness and death due COVID-19 placed the most vulnerable at an increased risk of multiple rights violations. The risk of violence against children, child labour, trafficking, and family separation increased significantly as a result.”[2]
While its effort may have had a positive impact on many children’s lives, it is only a drop in the ocean of suffering that too many children are drowning in.
“Across 129 countries in 2021, UNICEF-supported interventions reached 4.4 million children who had experienced violence (53 per cent are girls out of 2.3 million). This is an 80% increase from 2017… [at a cost of] US$773 million, including US$422 million for humanitarian action.”
The Global Report 2021 can be found by clicking here.
The unprecedented national responses to the COVID-19 pandemic did not only have an impact on the children living in the poorest countries, but they also impacted the lives of millions of children in the developed countries, including the US and the UK. According to the Guardian, there was an average of 669 child protection referrals a day in 2021 (because of incidents of domestic abuse) in England and Wales.[3] These are only cases where the police were involved, leaving many more isolated cases in the shadows.
“Police have warned that during the pandemic, many children were trapped in homes experiencing abuse and largely cut off from vital support networks during lockdowns.
“Several shocking cases were reported where toddlers and young children were killed despite social services being informed that they were in danger.”
Because experiencing domestic abuse can have a devastating impact on children, the NSPCC stated that it can decimate a child’s confidence and sense of security and can deeply impact their emotional well-being and mental health — even in later years, as an adult.
ACEs generally refer to traumatic experiences that occur to children aged 0-6. It is often assumed that because infants and young children lack ‘true’ consciousness and understanding of the world around them, their reactions may be different from older children's (also because they may not be able to verbalise their reactions to threatening or dangerous events) and that young age protects them from the impact of traumatic experiences.
A growing body of research dedicated to ACEs has established that young children can be affected by events that threaten their safety (or the safety of their parents/caregivers), and the impact on their lives (including symptoms) has been well documented. These traumas can be the result of intentional violence — such as child physical or sexual abuse, or exposure to domestic violence — or the result of natural disasters, accidents, sudden loss of a parent/caregiver, or war. Young children also may experience traumatic stress in response to painful medical procedures or chronic illnesses or highly-recurring infections.
The WHO estimates that:[4]
over 36% include emotional and physiological abuse (e.g., restriction of movement; patterns of belittling, blaming, threatening, frightening, discriminating against or ridiculing; and other non-physical forms of rejection or hostile treatment)
over 22% include physical abuse (hitting, beating, kicking, shaking, biting, strangling, scalding, burning, poisoning and suffocating, which may result in – or has a high likelihood of resulting in – harm to the child’s health, survival, development or dignity)
over 16% include neglect (e.g., failure to provide adequate nutrition, clothing, personal hygiene, supervision, and medical attention)
and sexual abuse, affecting twice as many girls (18%) than boys (7.4%). Sexual abuse is defined as the involvement of a child in sexual activity that he or she does not fully comprehend, is unable to give informed consent to, or for which the child is not developmentally prepared, or else that violates the laws or social taboos of society. Children can be sexually abused by both adults and other children who are — of the same age or at the same stage of development — in a position of responsibility, trust or power over the victim.
The WHO also estimates the cost of adverse childhood experiences totals $1.33 trillion each year (for North America and Europe only). The increased frequency in less developed countries may truly hide unreported cases of maltreatment and associated mental disorders the world around at all ages, including a lack of medical/psychological attention (and/or access to treatment)
While not all children go on to develop cPTSD or other types of mental ill-health, including eating disorders and behavioural (e.g., aggressiveness, addictions, substance misuse and more) and social inadequacies, addressing ACEs may be difficult and recovery may be very difficult in some cases (the more difficult the adverse childhood event is for the child, the greater the effect at the time and later in life if unresolved?)
So to answer the questions above,
ACEs have been linked to poor health in adulthood
The CDC has linked conditions like depression, asthma, cancer, and diabetes in adulthood to ACEs.[5]
In 2017, it estimated that 21 million cases of depression were linked to ACEs, 2.5 million cases of obesity and diabetes, and nearly 2 million cases of heart disease.
ACEs also increase the likelihood of heavy smoking and drinking and substance misuse, as well as poorer academic achievement and unemployment; therefore, the impact of ACEs can impact an adult in many different ways. It may even be greater in minorities including LGBTQ+ communities.[6,7]
ACEs have been linked to poorer physical health and risky health behaviours[8], poor mental health[9], and decreased life potential[10].
If it wasn’t enough,
ACEs are transgenerational
Studies show that, indeed, ACEs are often repeated in the same household and can be passed on to the next generation, as substance misuse and heavy alcohol consumption can lead to a repeated cycle, whereas an adult with unresolved trauma can repeat the same form of maltreatment on their children (including emotional and physical abuse).[11]
Living in a socially deprived neighbourhood or an environmentally hazardous environment (near a polluting factory, etc.) can also further exacerbate the risk of ACEs[12] and maladaptive personality types and levels of psychological distress[13].
In the same way, anxiety disorders and depression can often run in the same family, so can ACEs as a result of a multitude of factors, many of which are listed above.
It is thus important to break the cycle and protect your children.
This will be discussed, and solutions proposed, in a later article.
References:
CDC. (2014). Child Maltreatment. Facts at a Glance. Available at: https://www.cdc.gov/violenceprevention/pdf/childmaltreatment-facts-at-a-glance.pdf
UNICEF. (2021). Source: https://www.unicef.org
The Guardian. (2022). Domestic abuse: Average of 669 child protection referrals a day last year. Available at: https://www.theguardian.com/society/2022/feb/01/domestic-abuse-average-of-669-child-protection-referrals-a-day-last-year
WHO. (2014). Child maltreatment. Global estimates. Available at: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/4468
CDC. (2021. Adverse Childhood Experiences (ACEs). Preventing early trauma to improve adult health. Available at: https://www.cdc.gov/vitalsigns/aces/index.html#:~:text=ACEs%20are%20linked%20to%20chronic,cancer%2C%20and%20diabetes%20in%20adulthood.
Sanchez, O. (2022). Minority Stress — What is it and how does it affect communities. Available at: https://www.nutrunity.com/updates/minority-stress
Austin, A. Herrick, H. Proescholdbell, S. (2016). Adverse childhood experiences related to poor adult health among lesbian, gay, and bisexual individuals. American Journal of Public Health. 106, pp. 314-320, doi:10.2105/AJPH.2015.302904
Felitti, VJ. et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) study. American Journal of Preventive Medicine. 14(4), pp. 245–258.
Edwards, VJ. et al. (2003). . Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 160(8), pp. 1453–1460.
Metzler, M. et al. (2017). Adverse childhood experiences and life opportunities: Shifting the narrative. Children and Youth Services Review. 72, pp. 141–149.
Schofield, TJ. et al. (2018). Intergenerational continuity in adverse childhood experiences and rural community environments. American Journal of Public Health. 108, pp. 1148-1152, doi:10.2105/AJPH.2018.304598
Downey, L. Van Willigen, M. (2005). Environmental stressors: The mental health impacts of living near industrial activity. Journal of Health and Social Behavior. 46(3), pp. 289-305. doi:10.1177/002214650504600306.
Spinhoven, P. et al. (2016). Childhood maltreatment, maladaptive personality types and level and course of psychological distress: A six-year longitudinal study. Journal of Affective Disorders. 191, pp. 100–108. doi:10.1016/j.jad.2015.11.036